More than 200,000 Tricare beneficiaries, including 80,000 active-duty family members, will no longer be seen at 37 military health clinics across the country in the coming years, according to a Department of Defense report sent to Congress Wednesday.
The Pentagon is planning major changes to 50 military health facilities that will force many beneficiaries to find civilian doctors in their communities over the course of two to four years.
Assistant Secretary of Defense for Health Affairs Thomas McCaffery said Wednesday that the realignment supports the department’s effort to support the military health system’s return to focusing on troop health and military readiness.
According to the report Restructuring and Realignment of Military Medical Treatment Facilities, the clinics include Air Force, Army and Navy facilities. Two additional facilities will close and several others have already started transferring non-active duty beneficiaries to Tricare providers in surrounding communities.
The changes are part of a review of military hospital operations and Defense Health Agency administration required by Congress in the fiscal 2017 National Defense Authorization Act. As part of the largest transformation to the military health system since Tricare was introduced in 1992, Defense Health Agency is taking over management of all military hospitals and clinics while the military services are focusing their efforts to provide health services to military personnel.
The plan includes a reduction of roughly 18,000 uniformed medical personnel, with those retained focusing on the medical readiness and treatment of active duty personnel.
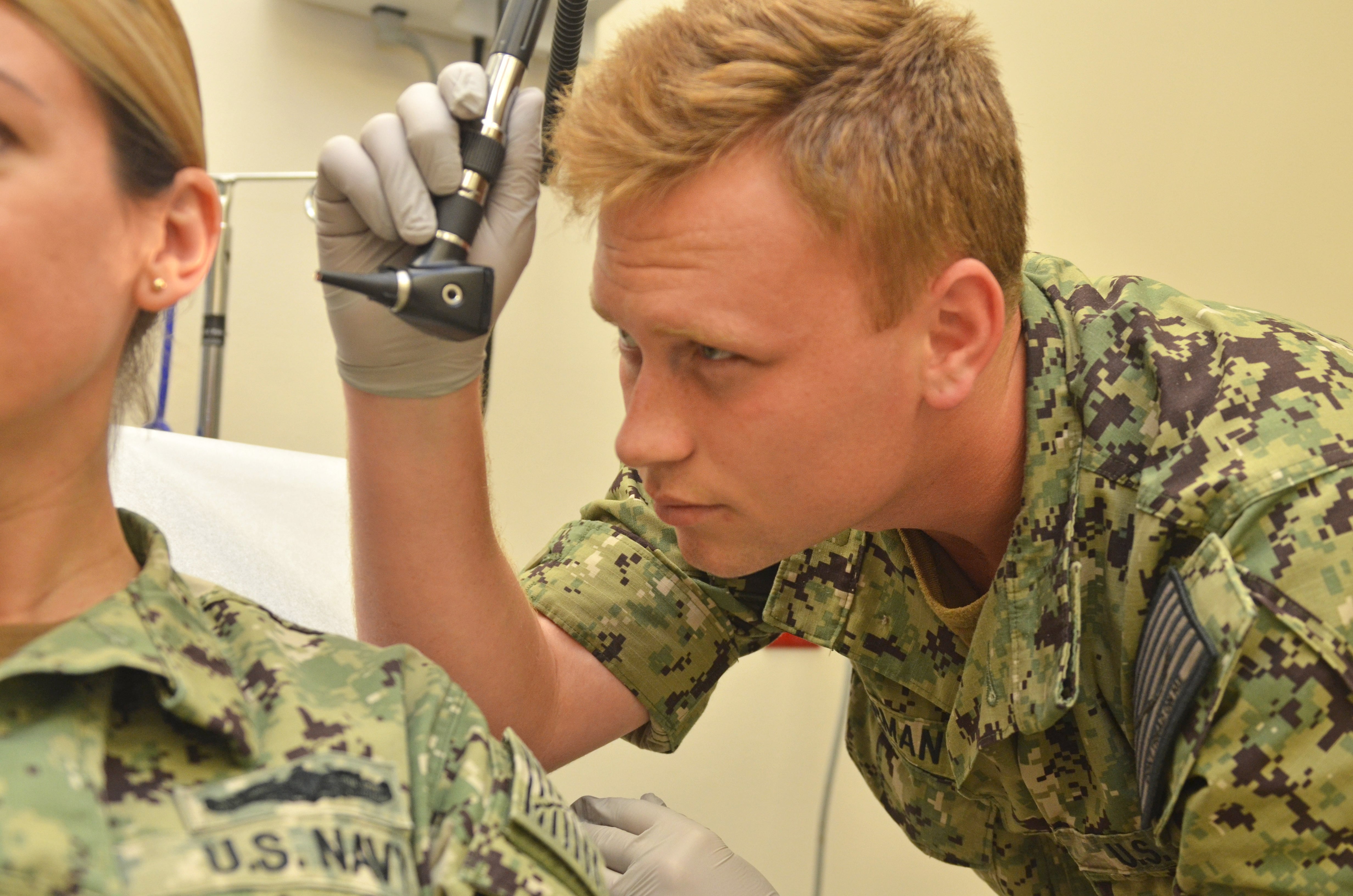
The idea is to ensure that military treatment facilities serve the troops and also perform as platforms to train military medical personnel in operational medicine, McCaffery told reporters Wednesday.
“That is what this review is about, and Congress recognized this as well: our military hospitals and clinics are first and foremost military facilities that exist with the primary focus on being the platforms by which we train our military providers to do their jobs, and ultimately ensure that our active duty get the care they need to make sure that they are medically ready to do their jobs,” McCaffery said.
The changeover should carry no additional out-of-pocket costs for active-duty family members who remain on Tricare Prime, other than pharmacy copayments should they decide to fill their prescriptions off-base.
RELATED
But military retirees and their family members will see their wallets affected by the switch, as they are required to make copayments and pay cost shares under the Tricare Prime and Tricare Select programs through civilian providers.
In their report to Congress, DoD officials acknowledged that some communities may have difficulties absorbing the new patient load. Late last year, House lawmakers complained that in locations like Seattle and San Francisco, family members were having issues finding civilian providers taking new patients.
But Pentagon officials said as demand grows, their Tricare contractors, Humana and Health Net Federal Services, will have to “increase network capacity” and they will work hard to “carefully manage” the transition.
"If, during implementation, local networks are challenged to absorb demand, the Department will revise its implementation plan,” they wrote.
For the latest report, DoD scrutinized operations at 343 facilities in the United States and selected 77 for additional review. Fifty were determined to be overhauled or close, including 37 clinics that now take all beneficiaries and eventually will only be open primarily to active duty personnel.
Seven of the 37 may continue to see active duty family members as space is available or if the military services determine that additional patients are needed to maintain providers’ skills. Also, beneficiaries will be able to continue using the pharmacies at the locations.
The report comes at a time when the Defense Health Agency is assuming management of all military treatment facilities, but McCaffery said the decisions were made by senior Department of Defense officials and are “not the result of DHA’s new responsibility.”
RELATED

The Department of Defense fiscal year 2021 budget projects an initial savings of $36 million from the changes — savings that will come from relocating military providers to other locations and purchasing care, often at discount prices, in the community.
“We have generally found that through our contracts that our care often is cheaper in the network from a government purchase point of view than the cost of actually doing it within our direct care system in some locations,” said Dr. Dave Smith, principal deputy assistant secretary of defense for health affairs. "But clearly of part of our methodology … the principle question was, are we getting readiness value out of this location? that is, is it worth the cost, if you will, compared to putting that [money] somewhere else in the system.”
Defense officials said they had not spoken with the soon-to-be affected beneficiaries but said they have spoken with leadership of the military treatment facilities in question to discuss the impact of changes on the local communities.
“This is basically our assessment of where we are making proposed changes, who are our enrolled beneficiaries in those markets in terms of the potential universe of beneficiaries to be impacted,” McCaffery said.
Here are the military health facilities expected to be affected by the changes. These facilities, while maintaining pharmacies for all beneficiaries, will transition to offer outpatient and occupational health services to only active-duty patients.
Air Force
17th Medical Group, Goodfellow Air Force Base, San Angelo, Texas
2nd Medical Group, Barksdale Air Force Base, Bossier Parish, La.
42nd Medical Group, Maxwell Air Force Base, Montgomery, Ala.
436th Medical Group, Dover Air Force Base, Del.
45th Medical Group, Patrick Air Force Base, Fla.
66th Medical Squadron, Hanscom Air Force Base, Mass.
6th Medical Group, MacDill Air Force Base, Tampa, Fla.
78th Medical Group, Robins Air Force Base, Warner Robins, Ga.
7th Medical Group, Dyess Air Force Base, Abiline, Texas.
87th Medical Group, Joint Base McGuire-Dix-Lakehurst, N.J.
Army
Army Health Clinic Barquist-Detrick, Frederick, Md.
Army Health Clinic Fillmore-New Cumberland, Fairview, Penn.
Army Health Clinic Fox-Redstone Arsenal, Huntsville, Ala.
Army Health Clinic Kenner, Fort Lee, Hopewell, Va.
Army Health Clinic Kirk, Aberdeen Proving Ground, Aberdeen, Md.
Army Health Clinic Rock Island Arsenal, Ill.
Joel Health Clinic, Fort Bragg, N.C. (currently under Defense Health Agency management)
Okubo Soldier Centered Medical Home, Joint Base Lewis McChord, Wash.
Army Health Clinic Southern Command, Fla. (Active duty foreign national military personnel will continue being accepted at the clinic. Their beneficiaries would be seen in the community.)
Navy
Naval Branch Medical Clinic Earle, Colts Neck, N.J.
Naval Branch Health Clinic Albany, Ga. (active duty family members may still be accepted on a space available basis).
Naval Branch Health Clinic Dalghren, Va.
Naval Branch Health Clinic Groton, Conn.
Naval Branch Health Clinic Indian Head, Md.
Naval Branch Health Clinic Belle Chasse, La.
Naval Branch Health Clinic, Naval Support Activity Mid-South, Tenn.
Naval Branch Health Clinic Portsmouth, N.H.
Naval Health Clinic Corpus Christi, Texas.
Naval Health Clinic New England, R.I.
Naval Health Clinic Patuxent River, Md.
Other changes:
633rd Medical Group Joint Base Langley-Eustis in Hampton, Va., is to transition to an ambulatory surgery center and outpatient clinic.
Army Health Clinic at Fort Eustis, Va., has already started the transition from an ambulatory surgery center to an outpatient facility.
Army Health Clinic Monterey, Calif., has transitioned to a primarily active-duty clinic with 96 non-active duty enrollees.
Munson Army Health Clinic at Fort Leavenworth, Kansas, has suspended its surgical capabilities.
Tripler Army Medical Center in Hawaii is being considered for recapitalization following additional market analysis.
Farrelly Army Health Clinic at Fort Riley, Kansas has already transitioned to serving only active duty and will remain so.
Fort Hood Medical Home, which closed in 2018 will continue serving as a sleep lab for Darnall Army Medical Center, Texas.
Naval Branch Medical Clinic Lakehurst, N.J. will become an occupational health, industrial hygiene and preventive medicine facility. Beneficiaries will be shifted to the network or other military facility.
San Onofre Marine Corps Branch Health Clinic will continue transitioning to an active duty-only clinic.
Kimbrough Ambulatory Care Center, Fort Meade, Md., will become an outpatient facility for all eligible beneficiaries.
Naval Hospital Beaufort, S.C., will become an ambulatory surgery center and outpatient clinic with beds to provide care for recruits outside the recruit recovery unit.
Naval Hospital Camp Lejeune, N.C. will continue to build its capabilities as the region’s Level II trauma center, taking military and civilian patients.
Robinson Army Medical Clinic at Fort Carson, Colo., will continue operating as an active-duty only clinic.
Closures:
The Family Health Clinic in Brandon, Fla., also known as the Sabal Park Clinic, will close after all patients are transferred to Tricare.
The North Columbus Community Based Medical Home at Fort Benning, Ga., will close.
Patricia Kime is a senior writer covering military and veterans health care, medicine and personnel issues.





